With little warning, two years ago Bob Kerby’s world dropped out of focus. It was as if someone had smeared Vaseline on the center of his glasses. Everywhere he looked was a blurred bull’s-eye. Reading, in particular, became a challenge. When he opened a book, words danced across the page in unpredictable patterns.
“I can see letters, but looking through the periphery you can’t interpret them,” the retired ND history professor says. “What you see is black squiggles on white. It drives you crazy, just crazy.”
Back in his teaching days, the military historian was legendary for the intricate battle maps he would draw on his classroom blackboard, marching armies across multicolor-chalked terrain, all rendered in detail. Today that would be a challenge.
Along with an estimated 5 to 10 million older Americans, including the novelist Stephen King and Notre Dame’s president emeritus Father Theodore Hesburgh, CSC, Kerby suffers from macular degeneration, an age-related eye condition that manifests as blurriness in the center of his field of vision.
The macula is a person’s “eye for detail,” that part of the retina responsible for visual acuity. Therefore, looking at a grid, someone suffering from macular degeneration would see a bunch of random wavy lines, possibly with sections blank or in shadow, explains Chicago ophthalmologist Dr. E. Michael Cassidy ’87. Those who suffer the condition also are likely to have trouble distinguishing colors, especially dark from light.
Some 10 percent of people ages 66 to 74 show signs of macular degeneration. The rate jumps to 30 percent for those 75 and above. Risk factors include smoking, high blood pressure, high cholesterol, obesity, high dietary fat and heredity. If a relative has been diagnosed, you have a 50-50 chance of getting it; the odds fall to one-in-eight if no one in your family has the condition.
“I’m one of the lucky ones,” Kerby says with a twist of gallows humor but no self-pity.
Macular degeneration damages the eyes of the unfortunate “lucky ones” in one of two ways. In the more slowly developing form, known as “dry” macular degeneration, cellular debris collects between the retina and the choroid, an area of the eye containing blood supply. Over time, the vision cells (known as the “rod” and “cone” photoreceptors) in the center of the macula essentially disintegrate, blurring the center of a person’s field of vision.
In the more aggressive “wet” version of the disease, abnormal blood vessels growing up from the choroid begin bleeding, causing irreversible scarring damage. The onset of “wet” macular degeneration usually is rapid and dramatic.
Kerby, in fact, has suffered from both forms of the disease, first being diagnosed with the dry form, which was controlled for many years. Then three years ago, he suffered a bout of “wet” macular degeneration. “It took about four weeks. It just got worse and worse over a short period,” he recalls. “By the time I got in to see a doctor my sight was pretty well gone. By then I had lost the capacity to read or drive.”
Today not a lot can be done to help those with the condition. Dry macular degeneration is treated most commonly with a vitamin/mineral regimen, consisting of such supplements as vitamins E and C, beta-carotene, copper, zinc and others that have been shown to aid in retarding the condition. The standard treatment for wet macular degeneration is to inject into the eye certain chemotherapy-type drugs that bind to the abnormal leaking blood vessels, destroying them, thus stopping the leaking and swelling.
“Unfortunately, all of this is mostly damage control, nipping something before it gets too extreme,” Cassidy says.
Clearly something more needs to be done.
- – -
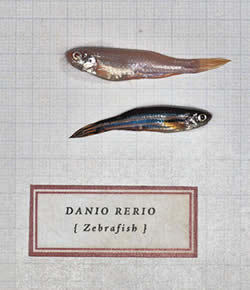
Swimming in a small tank of water, in a tiny Galvin Life Sciences basement room so brightly lit that it hurts your eyes, so brightly lit that a floor fan runs 24/7 to keep the lamp heat from cooking the occupants, are some remarkable fish whose fate, believe it or not, is connected to Bob Kerby’s.
“Swimming” may be an overstatement. These tiny, striped tropical fish, native to the streams of eastern India, are remarkable for what they are not doing. The zebrafish are not darting back and forth in the tank as one might expect. Instead, they hover in the water, nearly motionless. Bring your hand close to the glass and . . . nothing happens. They don’t scatter in panic. They stand their ground (stand their water?) because they don’t know any better. They are fearless because they, like Bob Kerby, are blind.
In the name of science, the fish got that way after an extended stay in total darkness followed by several days in the intensely lit room. Unlike Kerby, however, they will soon see again. Their eyes will naturally, spontaneously and mysteriously repair themselves. Within a month, the rod and cone photoreceptor cells will miraculously regenerate and the fish will be good as new, darting back and forth in full panic whenever anything moves anywhere near their tank.

Their eye-repair ability is of intense interest to Notre Dame’s David Hyde, a professor of biological sciences and the Kenna Director of the Center for Zebrafish Research. In one form or other, Hyde has been studying eye problems throughout his 30-plus-year career, first using the lowly fruit fly as a model system, then switching over to zebrafish 17 years ago.
Zebrafish offer several research advantages, Hyde says. First, they are vertebrates, a higher level organism than the fruit fly, and therefore their eye is more like the human eye. Zebrafish also develop fairly quickly, taking about three months to reach maturity. Since their eggs are fertilized outside of the female, genetic manipulation is easy.
“On top of that, their embryos are transparent, so you can easily see the development of the internal organs. When you manipulate genes you can easily see how it perturbs their development,” Hyde says.
The Notre Dame biologist has long been intrigued by “what if” questions. The most interesting research questions, he has found, often are those that begin “What if . . .” and end in “Why not?” Those are the great ones, the questions that unlock hope and open the door to possibility. They are the ones that drive progress.
A seminal experiment 15 years ago that ended with one such “what if?/why not?” question has set the course for Hyde’s work ever since and is largely the reason the tank of blind zebrafish described previously, as well as 2,000 other tanks holding 80,000 of their “cousins,” now rest in the basement of Galvin.
“Not long after we set up our lab with zebrafish as a model system, we decided to study retinal damage using genetic means,” the biologist recalls. In one of their first experiments the ND researchers employed the “bright light” method to damage the zebrafish retinas, but they couldn’t do it. When they checked, the researchers were stunned to see the little striped fish flitting around normally with no visual impairment. That could mean one of two things: Either they had super zebrafish with preternatural powers, or they were doing something wrong.
Actually, there was a third possibility: The fish were only temporarily blind. That’s precisely what Hyde and his crew found when they examined the fish earlier in the experiment timeline: The zebrafish had been regenerating so fast that the researchers were missing the changes.
“We knew that some regeneration would go on,” Hyde says, “but we thought it would be extremely slow, as others had shown with goldfish.” (Goldfish take six to nine months to repair their retinas, whereas Hyde’s group had just discovered zebrafish fixing their eyes in less than a month.)
On further analysis, Hyde and his associates concluded that a band of cells in the eye known as Müller glia were responsible for regenerating the eye’s rod and cone photoreceptor cells. Subsequently, the cells were identified as adult stem cells, namely cells that have the uncanny ability to change from an undifferentiated cell into a specialized cell, such as bone, nerve or muscle.
The ND biologists found that when the fish eye senses retinal damage, the Müller cells, which normally support cells within the eye, are triggered to divide and migrate to the retina, where they are transformed into photoreceptor cells, replacing the damaged ones.
The finding led Hyde to wonder if people could repair their eyes like zebrafish. And why not? Precisely what are the biochemical reactions that trigger the repair? If someone could figure out how the zebrafish manages the trick, the key genes involved and the biochemical pathways, that information might lead to cures for macular degeneration as well as a host of other retinal diseases.
“I’m fairly convinced that what we see when the human retina gets damaged is similar with what we see in the fish retina, up to a point,” Hyde says. “But there is some reason why the human retina won’t regenerate. It’s as if it wants to. It recognizes that there is damage. The [human] Müller glial cells start to proliferate, but then the next step, which is to determine precisely which cells are missing, that doesn’t happen.”
In fact, what happens is the last thing anyone would want: Human glial cells start migrating to abnormal places in the retina. Instead of fixing the eye, the migrating cells cause more damage, known as “glial scarring.” They make a bad situation worse.
Precisely why the fish eye responds to retinal damage by regenerating a functional retina while the human eye creates more damage remains a mystery for Hyde and others to solve.
Like most things in nature, the mystery is mind-numbingly complex. You don’t just directly tweak the rods and cones and immediately see again, Hyde says. To regain clear, sharp sight requires fixing a host of complicated, multilayered, interlocking, intermediate processes that eventually effect the cure.
After identifying the Müller glia as the source of adult stem cells that repair the zebrafish retina, Hyde and his colleagues ratcheted up their work to identify the molecules which are important in the process. To do that, they began looking at “gene expression” changes.
Using a technique known as “micro-array analysis,” Hyde’s lab, which in essence is a little company with 20 employees, has identified several thousand zebrafish genes involved in repairing retinal damage. When an injury occurs, genes, which are templates for the production of proteins, the building blocks of the body, are activated, causing the eye to produce the specific proteins charged with repairing the eye.
Working on another track at about the same time, the ND biologists found that when they selectively killed certain zebrafish eye cells, only those specific types would regenerate. They concluded that each dying cell, therefore, must produce a cell-specific chemical cue that triggers its replacement. These chemical cues “tell” the eye an injury has occurred as well as which types of cells are injured and where they are located.
“We realized then and there that just looking at dying photoreceptors isn’t going to give us the whole story,” Hyde says. “So we started developing additional zebrafish model systems, which we could use to do comparisons that subsequently have proven to be very important.”
The comparison studies allowed Hyde and his colleagues to determine which of the triggers are specific and which are more broadly based.
“And then we did an experiment which I’d been hinting to the lab for a year that we should try,” Hyde says. Essentially the experiment involved damaging a fish’s retina and isolating all the proteins from that retina, which subsequently would be injected into a healthy fish eye. “The thinking was if we do that, we should induce a regeneration response in the healthy retina.
“That was a key experiment. It allowed us to identify molecules, such as Tumor Necrosis Factor Alpha (TNF-alpha) and others, that appear very early in the whole response but weren’t showing up in the gene micro-array study.”
Hyde and his colleagues found that TNF-alpha is a cell-specific protein produced in the dying photoreceptor cells. Therefore, they concluded it must play some critical role in initiating the repair response. The dying rods and cones release the protein, then the Müller cells chemically “recognize” it and start the retina repair process.
Currently, Hyde’s group is focusing on several of these regeneration proteins, some of which, like TNF-alpha, are produced only in response to the injury of a specific cell type. Others, such as a protein called STAT3, are triggered more broadly and elicit a broader response.
Hyde has found that STAT3 exists in glial cells at very low levels before injury. Once the retina is damaged, however, the level of STAT3 shoots way up. “It responds very quickly to injury. It binds with DNA, regulating gene expression. It is broad-based, a molecule that can affect anywhere from 10 to 100 different genes.”
It also is a prime example of just how complicated and interlocking the retinal repair process is. For instance, to become activated it requires another molecule in the cell membrane, and that molecule requires an outside protein to bind to it. Hyde and his colleagues suspect the “outside protein” that unlocks the process is none other than TNF-alpha, which the dying photoreceptors produce.
The ND professor likens his retinal research to solving a gigantic jigsaw puzzle. “First you have to find the piece and then you have to find where it fits. You might look at all those pieces and feel overwhelmed. But if you can find a couple of the edges, then you can build off those.
“Once you get a handle on some of these molecules then you can make certain predictions, hypothesize how they fit into the process. You can see broadly what the pattern is. So, for instance, if you see ‘a’ and ‘b,’ then you might conclude that ‘c,’ which is related to both of these, also may be important, [such as the relationship between TNF-alpha and STAT3]. Working like that, you can begin to deduce components in the process.
“We may have 5 percent of the picture today — it’s hard to say,” he says. “But compared to where we were two or three years ago, it’s fantastic. Then it was next to nothing. We’ve learned so much in such a short span of time.”
This past spring Hyde added an exciting new line of inquiry that he believes has an excellent chance of helping people sooner rather than later.
“We aren’t dropping the zebrafish work,” he says. “The potential for regenerating neurons, which could result in a total cure, is still high — although perhaps 10 to 15 years away.”
Hyde’s new direction, aimed at the near term, is born in part from his frustration at not yet having any help for those currently suffering from retinal disease. “Every week I receive emails from people all over the country who say they suffer from macular degeneration and ask to volunteer for a clinical trial, and I have to write back and say there’s nothing we can do just yet,” he laments.
That soon may change.
Not long ago, after reading about an English research team that had successfully coaxed embryonic stem cells into becoming retinal pigment epithelial (RPE) cells, Hyde saw a promising new avenue for his lab. The specialized RPE cells are crucial to the life of photoreceptors; if they die, the rods and cones die as well. He understood that if you can restore RPE cells, you have the basis for a treatment for macular degeneration as well as several other diseases.
When Hyde learned that the English researchers had begun a clinical trial last summer using their cultured RPE cells injected into the diseased eyes of volunteers with macular degeneration, he decided to explore the technique, but using adult stem cells instead of embryonic ones.
That slight but significant change will, he believes, solve two vexing problems. First, the use of adult stem cells means all ethical objections to the therapy are removed.
The second problem relates to the tiny percentage of cells produced from the embryonic stem cells that are not RPE cells. “It’s unclear what these cells are,” Hyde says, “but if they remain as embryonic stem cells, they may proliferate and cause a tumor, and that would be devastating.”
The ND biologist hopes to circumvent this problem by using adult stem cells. Hyde explains that unlike embryonic stem cells, which are unlimited in the type they may become, adult stem cells are confined to a few forms. Therefore, it’s believed their limited nature makes them less likely to produce a tumor. In fact, in countless experiments using adult stem cells, no tumor has ever been reported forming.
Hyde’s team now is ramping up work on the project, gathering stem cells from bone marrow, fat tissue and umbilical-cord blood to see if any of these sources may yield viable RPE cells.
“It seems to me this is something that can move very quickly from first demonstrating that we can produce RPE cells from adult stem cells, then moving to clinical trial,” he says. “This may not restore vision, but it likely can block further loss of vision and would be a huge advance in therapy, offering hope where there has been none.”
John Monczunski is a freelance writer and a former associate editor of this magazine.
Learn more about Professor Hyde’s research and about Notre Dame’s Initiative on Adult Stem Cell Research and Ethics.